Parkinson’s disease is a neurodegenerative disorder that affects millions of people worldwide. It is characterized by the progressive loss of dopamine-producing cells in the brain, leading to symptoms such as tremors, stiffness, and difficulty with movement and coordination. While there is currently no cure for Parkinson’s, researchers are constantly exploring new avenues for treatment and management of the disease.

One such avenue is the use of glutathione.
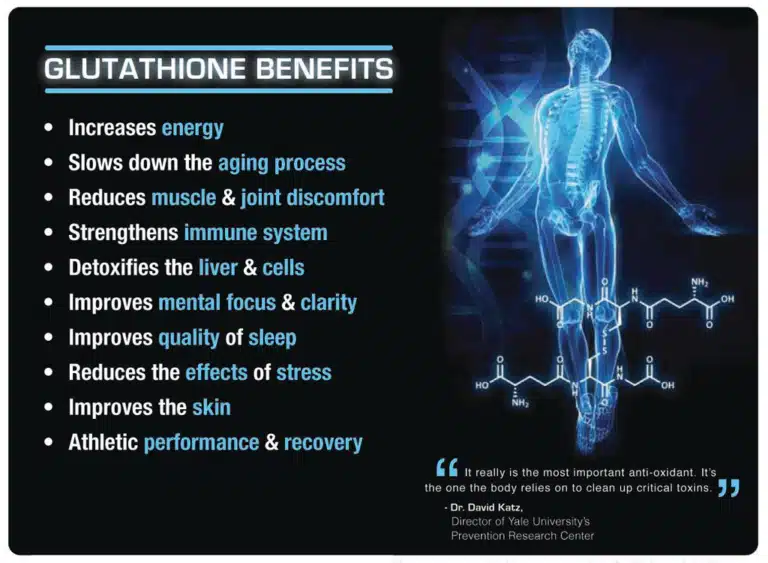
Glutathione is a powerful antioxidant that is naturally produced by the body. It plays a crucial role in protecting cells from oxidative stress and damage caused by free radicals. In recent years, there has been growing interest in the potential benefits of glutathione for Parkinson’s disease.
Studies have shown that individuals with Parkinson’s disease have lower levels of glutathione in their brains compared to healthy individuals. This deficiency may contribute to the oxidative stress and inflammation that are characteristic of the disease. By increasing glutathione levels, it is believed that we can potentially reduce the progression of Parkinson’s and alleviate some of its symptoms.
One way to increase glutathione levels is through the use of supplements. Oral glutathione supplements are available, but their effectiveness is still a topic of debate. The main challenge with oral supplementation is that glutathione is broken down in the digestive system before it can reach the brain. However, there are alternative methods of administration that have shown promise.
Intravenous (IV) administration of glutathione bypasses the digestive system and delivers the antioxidant directly into the bloodstream. This method has been found to increase glutathione levels in the brain and improve symptoms in some individuals with Parkinson’s disease. However, more research is needed to determine the optimal dosage and long-term effects of IV glutathione therapy.
Another approach to increasing glutathione levels is through the use of precursors or building blocks of glutathione. These precursors, such as N-acetylcysteine (NAC) and alpha-lipoic acid (ALA), can be taken orally and are converted into glutathione in the body. Studies have shown that NAC supplementation can increase glutathione levels and improve motor symptoms in individuals with Parkinson’s disease.
In addition to supplementation, lifestyle factors can also influence glutathione levels. Regular exercise, a healthy diet rich in fruits and vegetables, and adequate sleep have all been shown to support glutathione production. Avoiding exposure to toxins and reducing stress levels can also help preserve glutathione levels in the body.
While the potential benefits of glutathione for Parkinson’s disease are promising, it is important to note that more research is needed to fully understand its effectiveness and safety. Parkinson’s is a complex disease with various underlying factors, and glutathione is just one piece of the puzzle.
It is also worth mentioning that glutathione is not a cure for Parkinson’s disease. It may help alleviate some symptoms and slow down the progression of the disease, but it cannot reverse the damage already done to the brain.
Furthermore, it is crucial to consult with a healthcare professional before starting any new treatment or supplementation regimen. They can provide personalized advice based on your specific condition and medical history.
In conclusion, glutathione shows potential as a therapeutic option for Parkinson’s disease. Its antioxidant properties and ability to reduce oxidative stress make it an intriguing avenue for further research. However, more studies are needed to determine the optimal dosage, administration method, and long-term effects of glutathione therapy. In the meantime, individuals with Parkinson’s disease can focus on maintaining a healthy lifestyle and discussing potential treatment options with their healthcare team.
References
1. Jenner P. Oxidative stress in Parkinson’s disease. Ann Neurol. 2003;53 Suppl 3(Suppl 3):S26-S36. doi:10.1002/ana.10483
2. Hauser DN, Hastings TG. Mitochondrial dysfunction and oxidative stress in Parkinson’s disease and monogenic parkinsonism. Neurobiol Dis. 2013;51:35-42. doi:10.1016/j.nbd.2012.09.015
3. Smeyne M, Smeyne RJ. Glutathione metabolism and Parkinson’s disease. Free Radic Biol Med. 2013;62:13-25. doi:10.1016/j.freeradbiomed.2013.05.001
4. Sian J, Dexter DT, Lees AJ, et al. Alterations in glutathione levels in Parkinson’s disease and other neurodegenerative disorders affecting basal ganglia. Ann Neurol. 1994;36(3):348-355. doi:10.1002/ana.410360305
5. Monti DA, Zabrecky G, Kremens D, et al. N-acetyl cysteine may support dopamine neurons in Parkinson’s disease: preliminary clinical and cell line data. PLoS One. 2016;11(6):e0157602. doi:10.1371/journal.pone.0157602
6. Magalingam KB, Radhakrishnan A, Haleagrahara N. Protective mechanisms of flavonoids in Parkinson’s disease. Oxid Med Cell Longev. 2015;2015:314560. doi:10.1155/2015/314560
7. Smeyne RJ, Breckenridge CB, Beck M, et al. Assessment of the effects of MPTP and paraquat on dopaminergic neurons and microglia in the substantia nigra pars compacta of C57BL/6 mice. PLoS One. 2016;11(6):e0157177. doi:10.1371/journal.pone.0157177
8. Shults CW, Haas RH, Passov D, Beal MF. Coenzyme Q10 levels correlate with the activities of complexes I and II/III in mitochondria from parkinsonian and nonparkinsonian subjects. Ann Neurol.